
My New Frustration – U.S. Health Care (or lack there of?)
March 10th, 2021 - By Patrick T. McBriarty
My frustration now has a new focus. The crying shame of the U.S. medical establishment is resistant to recognizing Ivermectin as a remedy to mild, severe, and long-Covid-19 symptoms — particularly as huge segments of the population wait for vaccines and continue to get sick and many die.
There is a lot of good information to share with doctors about Ivermectin. Certainly, IVM may not work for everyone, but with little or no side effects and the potential upside against Covid-19 why not try it?

One serious caution with IVM is for people with a compromised brain-blood barrier such as Meningitis. In other words if you have a compromised brain-blood barrier like Meningitis – estimated 1.2 million cases worldwide each year — don’t take Ivermectin. The other lesser issue being discussed on social media is after taking IVM daily for 2-4 weeks or more people struggle with inflammation after coming off IVM. Several groups are sharing information trying to figured this out. Luckily my symptoms are pretty mild though pernicious and hopefully will not be taking IVM more than a few more days and avoid that problem.
 The Bigger problem is… IVM is way cheap! Yes, that’s right being inexpensive means Big Pharma or Big Health Care cannot make money on this treatment. As the movie Wall Street is quoted, “GREED is good!” There is little monetary incentive or business reason to encourage the use of IVM against Covid-19. And worse Big Pharma and Big Health Care representative may see this as a threat and sew doubt, objections, and controversy around the use of IVM to keep more expensive and less effective treatments in the forefront to generate income and allow the health care industry to continue to cash in. My first round of IVM cost $26 plus $20 for shipping and handling.
The Bigger problem is… IVM is way cheap! Yes, that’s right being inexpensive means Big Pharma or Big Health Care cannot make money on this treatment. As the movie Wall Street is quoted, “GREED is good!” There is little monetary incentive or business reason to encourage the use of IVM against Covid-19. And worse Big Pharma and Big Health Care representative may see this as a threat and sew doubt, objections, and controversy around the use of IVM to keep more expensive and less effective treatments in the forefront to generate income and allow the health care industry to continue to cash in. My first round of IVM cost $26 plus $20 for shipping and handling.
In the U.S. we are all about making money, and the U.S. health care system is no different. The U.S. health care industry and health insurance is organized on a fee-for-service basis. No shoes, no shirt, no health insurance? No service! Money is the incentive driving health care. Direct financial incentives should be tied to improving the health and wellness of the U.S. population not fees for service. The illogical health care system is perpetuated helping to drive the growth of the U.S. economy. There is little incentive to change the system because more expensive health care and insurance industry feeds the economy and besides patient outcomes are not well tracked or publicized. Financial incentives drive doctors, hospitals, and clinics to run tests, prescribe drugs, create expensive vaccines, technology, procedures, and make decisions biased toward generating income with little or no financial incentives to improve patient outcomes. Again financial incentives should be designed to push for patient health and wellness but patients are left as individuals to fight the system with no one to advocate for them.
incentives should be tied to improving the health and wellness of the U.S. population not fees for service. The illogical health care system is perpetuated helping to drive the growth of the U.S. economy. There is little incentive to change the system because more expensive health care and insurance industry feeds the economy and besides patient outcomes are not well tracked or publicized. Financial incentives drive doctors, hospitals, and clinics to run tests, prescribe drugs, create expensive vaccines, technology, procedures, and make decisions biased toward generating income with little or no financial incentives to improve patient outcomes. Again financial incentives should be designed to push for patient health and wellness but patients are left as individuals to fight the system with no one to advocate for them.
 Of course this is complicated by insurance companies situated between the patient and health care provider. As for-profit businesses insurance companies make money by collecting and holding money which is then invested to generate additional returns and profits. So insurance company decisions to deny service, delay payments, or disqualify procedures add to the bottom line, while the individual patient’s health and well being is rarely a secondary consideration.
Of course this is complicated by insurance companies situated between the patient and health care provider. As for-profit businesses insurance companies make money by collecting and holding money which is then invested to generate additional returns and profits. So insurance company decisions to deny service, delay payments, or disqualify procedures add to the bottom line, while the individual patient’s health and well being is rarely a secondary consideration.
I am not implying some kind of conspiracy nor collusion. I am saying the U.S. health care and health insurance system is not designed to help patients. Financial incentives of the system leave the best interest of the patient and U.S. population on the sidelines. That ought to be changed. Life threatening conditions are generally managed by U.S. health care, however long-term ailments, chronic pain, and difficult diseases like Lupus, ME/CFS or cancer leave patients and their families to face a frustrating labyrinth to get help from the U.S. health care and insurance system standing between you and effective treatments. Again with no or poor health insurance patients are left to God, Allah, the greater good, or their own devices to try and muddle through.
U.S. doctors call their work practicing medicine (author’s emphasis on “practice”). Doctors are trained not to break the rules or employ holistic or alternative medicine even if it is effective and easy to implement. Doctors carry burdensome and expensive malpractice insurance and must play it safe or risk litigation and even threats by health care administrators or insurance companies of losing  malpractice insurance. Therefore U.S. doctors rarely dare step outside normal medical practices and truly work with patients to try a medicine or practice not backstopped by published triple-blind, gold-standard medical trials or definitive research (which is very expensive). Given the specter of astronomical malpractice settlements few doctors can afford to practice without malpractice insurance let alone try something new or untried? These constraints impact individual medical treatment and resist implementing continuous improvement of medical practices or treatments.
malpractice insurance. Therefore U.S. doctors rarely dare step outside normal medical practices and truly work with patients to try a medicine or practice not backstopped by published triple-blind, gold-standard medical trials or definitive research (which is very expensive). Given the specter of astronomical malpractice settlements few doctors can afford to practice without malpractice insurance let alone try something new or untried? These constraints impact individual medical treatment and resist implementing continuous improvement of medical practices or treatments.
Meanwhile in a pandemic these issues are magnified as more and more people suffer and die. In the U.S. alone we surpassed a half-million deaths attributable to Covid-19. Shouldn’t we try something different?
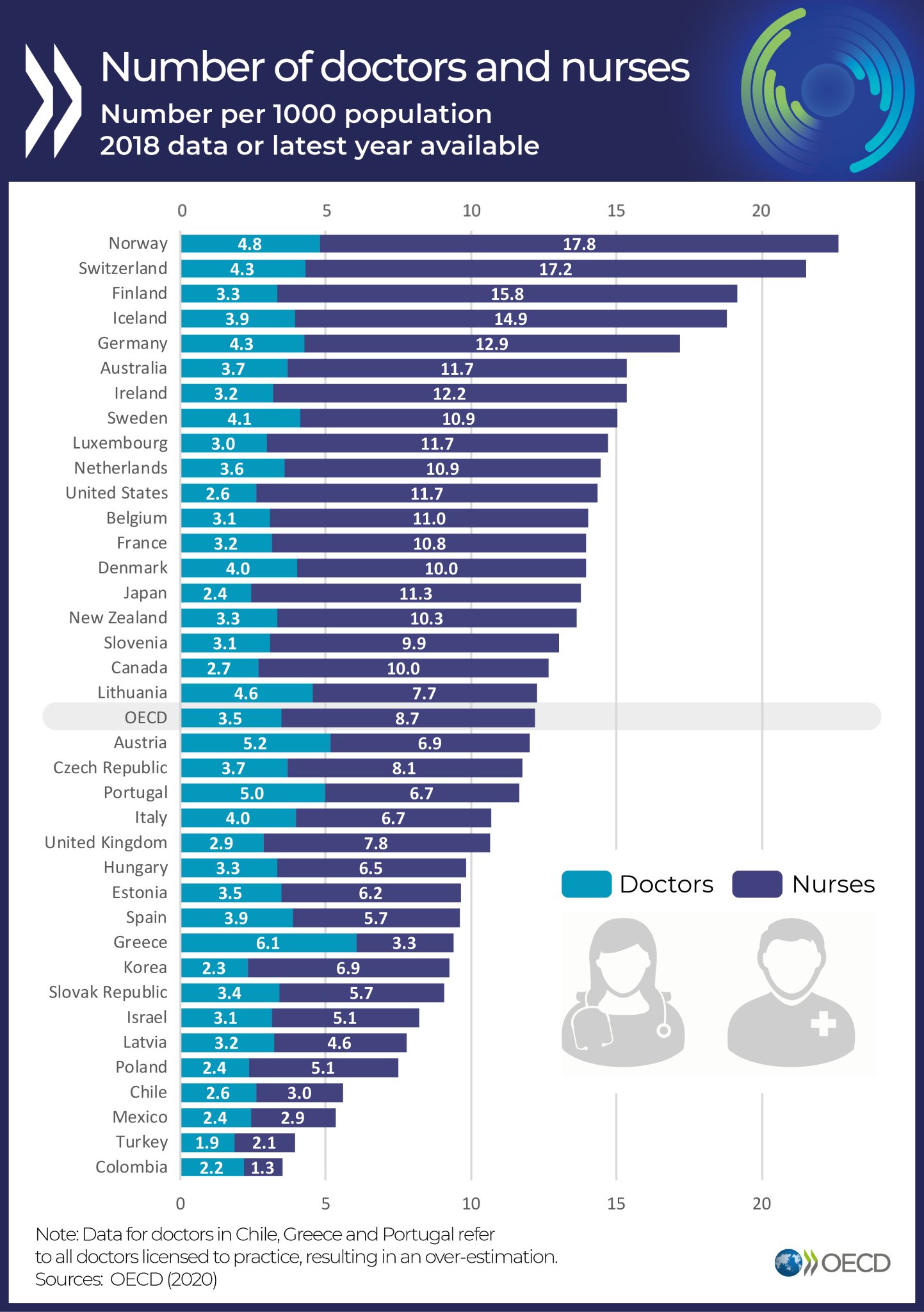
As both an indictment of the U.S. health care system and sad state of affairs the U.S. by far spends more per person on health care than any country on earth. Yet, as a proxy for national health in the United States, life expectancy at birth in 2019 was 78.5 years, while other developed countries spend substantially less per capita their populations and live 2-6 years longer than we do. Checkout life expectancy data from the World Health Organization in years below:
-
- Australia — 83.04
 Canada — 82.24
Canada — 82.24- Denmark — 81.32
- Finland — 81.61
- France — 82.48
- Ireland — 81.84
- Italy — 82.62
- Japan — 84.26
- Netherlands — 81.79
- New Zealand — 81.96
- Norway — 82.62
- Singapore — 83.22
- Spain — 83.22
- Sweden — 82.4
- Switzerland — 83.45
- United Kingdom — 81.4
Our frontier spirit and cowboys story most Americans tell ourselves is hurting us, as we regularly ignore useful ideas from clever people living in other countries. These are discounted out of hand often simply because they were not invented here first. Combine this with xenophobia, our bias against less developed countries, and racism how can a thoughtful American reasonably expect the United States to ever improve let alone adopt effective changes in health care — let alone other broken national systems like: education, policing, or taxation. God forbid we honestly compare and contrast ourselves with other nations. Country comparisons are healthy and helpful to spur innovation and better ways to live but change must just be too hard for America.
 So, “God forbid,” as the anti-vaxxers might say to the U.S. medical system about trusting foreign doctors, particularly from less developed countries experienced in the use and efficacy of Ivermectin. “Object and spread fear to bury the facts,” as representatives of Big Pharma might say to keep public from learning three scientists (Campbell, Satoshi, and Tu) discovered Ivermectin in 1975 and won a noble prize for their work. “Ignore, ignore, ignore,” doctors more beholden to corporate profit than public health even though more than 4 billion doses of IVM administered to date combating tropical diseases (like scabies or river blindness) have had little or no adverse side effects. Add to this July’s tweet, “62 studies confirm the effectiveness of hydroxychloroquine,” from our past President since quashed by the media as inaccurate and false of course scientists and policy folks are even more resistant to successful off-the-shelf prescriptions to relieve the suffering and death of Covid-19.
So, “God forbid,” as the anti-vaxxers might say to the U.S. medical system about trusting foreign doctors, particularly from less developed countries experienced in the use and efficacy of Ivermectin. “Object and spread fear to bury the facts,” as representatives of Big Pharma might say to keep public from learning three scientists (Campbell, Satoshi, and Tu) discovered Ivermectin in 1975 and won a noble prize for their work. “Ignore, ignore, ignore,” doctors more beholden to corporate profit than public health even though more than 4 billion doses of IVM administered to date combating tropical diseases (like scabies or river blindness) have had little or no adverse side effects. Add to this July’s tweet, “62 studies confirm the effectiveness of hydroxychloroquine,” from our past President since quashed by the media as inaccurate and false of course scientists and policy folks are even more resistant to successful off-the-shelf prescriptions to relieve the suffering and death of Covid-19.
So, a lopsided debate has been running for months below the surface of mainstream media on the efficacy of Ivermectin. Social media is filled with users in multiple groups comparing notes, experiences, symptoms, and remedies in an effort to find relief to their suffering seeking a path to full health. What I and others have learned experimenting in parallel with new data and continuing release of new studies showing the efficacy of Ivermectin is it works. The case is compelling particularly as the risks are low. Marginal enough for me, as an athlete and proponent of healthy living, to try it without a prescription. It helped end 350-days of undiagnosed suffering.
What will it take for more Americas to wake up and begin asking questions? We have to recognize sitting back and hang our hopes on vaccines alone to solve the SARS-CoV-2 pandemic is foolish. As time slips by this disease will continue to mutate and change and we will need a variety of methods both simple and complex in our collective arsenal to move forward. The best of these may be simple: masks, fresh air, selective quarantines, contact tracing, and better ventilation in buildings. However medical treatments besides vaccines like the I-MASK+ protocol employing Ivermectin, other prescriptions, and vitamins can combat and defeat this virus.
A Few Links to Research & Stories on Ivermectin:
-
“How a nurse saved herself from her battle with COVID-19,” on YouTube, posted March 11, 2021.
- “Ivermectin and COVID: what’s going on? (Dr. Carlos Chaccour, ISGlobal)” on YouTube, posted March 8, 2021 offers a great review of the history with this issue from its beginning to current time.
- FLCCC Alliance Weekly Update – Possible Solutions for Long Haulers (Feb. 17, 2021) This is the FLCCC Weekly Update regarding possible solutions for those with Long Haulers.
- “Sharp reduction in COVID-19 case fatalities and excess deaths in Peru in close time conjunction, state-by-state, with ivermectin treatments,” by Quintero, Hibberd, and Scheim, on SSRN website, posted: 21 Jan. 2021. On May 8, 2020, Peru’s Ministry of Health approved ivermectin (IVM) for the treatment of COVID-19. A drug of Nobel Prize-honored distinction, IVM has been safely distributed in 3.7 billion doses worldwide since 1987. It has exhibited major, statistically significant reductions in case mortality and severity in 11 clinical trials for COVID-19, three with randomized controls. The indicated biological mechanism of IVM is the same as that of antiviral antibodies generated by vaccines—binding to SARS-CoV-2 viral spike protein, blocking viral attachment to host cells.
- FLCCC Alliance – The Front Line Covid-19 Critical Care Alliance is an international collective highly published critical care specialists from major academic medical centers with collectively over 1,000 medical publications started in January 2020 to studying SARS-Cov-2 finding solutions. Their recommendations are based on the rapidly emerging research into COVID-19, the early clinical experience in China reflected by the Shanghai expert commission, and their decades-long clinical and research experiences in severe infectious diseases around the United States.
- FLCCC Alliance’s FAQs on Ivermectin, last updated Feb. 15, 2021
- “What’s Behind the Ivermectin-For-Covid Buzz?” by Kristina Fiore for MedPage Today, Jan. 6, 2021, provides a good report on the back and forth between the FLCCC Alliance and medical establishment’s arguments. Interestingly there are no comments or discussion from patients here.
- “COVID-19 IVERMECTIN Saved Lives in Toronto Nursing Home,” June 22, 2020, YouTube video. Discusses Scabies treatment of Ivermectin in Canada and its positive effects on preventing Covid at a nursing home.
- “COVID-19 in Nursing Homes: a Way Forward to End the Tragedy,” by Covexit.com, Dec. 4, 2020. This article presents a concrete way forward for avoiding or at the very least containing COVID-19 outbreaks in nursing homes, through prophylaxis and early treatment.
- “Oral ivermectin for scabies outbreak in long-term care facility: potential value in preventing COVID-19 and associated mortality,” by Bernigaud, Guillemot, Ahmed-Belkacem, Brimaldi-Bensouda, Lispine, Berry, Softic, Chenost, Do-Pham, Giraudeau, Fourati, and Chosidow, in British Hournal of Dermatology, 16 January 2021. Tells of patients treated with ivermectin for scabies had significantly less infections and no mortality from Covid.
- “A five-day course of ivermectin for the treatment of Covid-19 may reduce the duration of the illness,” by Ahmed, Karim, Ross, Hossain, Clemens, Sumiya, Phur, Rahan, Zaman, Somani, Yasmin, Hasnat, Kabir, Aziz in the International Journal of Infectious Diseases, Feb. 1, 2021.
- “Use of Ivermectin Is Associated With Lower Mortality in Hospital Patients With Coronavirus Disease 2019,” by Juliana Rajter, Sherman, Fatteh, Vogel, Sacks, and Jean Rajter in CHEST Journal, Jan. 1, 2021.
